Richfield (435) 896-6497
Ephraim (435) 283-4076
October 2023
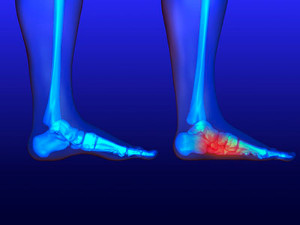
Causes, Symptoms, and Treatment of Poor Blood Circulation in the Feet
Poor blood circulation in the feet and legs is often caused by peripheral artery disease (PAD), which is usually the result of a buildup of plaque in the arteries. Plaque buildup, or atherosclerosis, can be the result of excess calcium and cholesterol in the bloodstream. This restricts how much blood can flow through arteries. Reduced blood flow to a certain area of the body severely limits the amount of oxygen and nutrients that part of the body receives. This leads to degeneration in the muscles and other tissues. Sometimes, poor blood circulation in the feet and legs can be caused by other conditions, such as the damaging or inflammation of blood vessels, known as vasculitis.
The lack of oxygen and nutrients caused by poor blood circulation can restrict muscle growth and development, as well as cause muscle pain and cramps, weakness, and stiffness. Other common symptoms include numbness in the legs and feet, skin discoloration in the affected limbs, slower nail and hair growth, and erectile dysfunction in men. In more severe cases of PAD, pain can be present even when a person isn't exercising, and may range from mildly uncomfortable to completely debilitating.
Poor blood circulation in the feet and legs is more common in those who are overweight or obese, have diabetes, high blood pressure, high cholesterol, who smoke, or who have a family history of PAD or related conditions such as a heart attack, stroke, etc. Diabetes and smoking place a person at greatest risk for developing poor blood circulation, although advanced age, over 50, can also increase risk.
If you are experiencing poor blood circulation in the feet and legs caused by PAD, it is important to make changes to your lifestyle in order to reduce your risk of experiencing a heart attack or stroke caused by this condition. If you smoke, quit completely. This will increase the amount of oxygen in your bloodstream. Exercising and reducing the saturated fats in your diet. Saturated fats come from fatty meats, fried foods, whole milk, etc., can make a difference in improving blood circulation in feet. It is also important to avoid developing influenza and to carefully control your blood sugar if you have diabetes.
Your doctor may recommend combining lifestyle changes with a prescription medication regimen to improve blood circulation. The most commonly-used medications for PAD are called statins and work by blocking the amount of enzymes in your body that produce cholesterol. They are known by the brand names Zocor, Lipitor, Crestor, and others.
Definition and Common Causes of Poor Circulation

Poor circulation, a medical condition also known as circulatory insufficiency, refers to the inadequate flow of blood through the blood vessels, impairing the distribution of oxygen and nutrients to the body's cells and organs. The feet are often affected, leading to a variety of symptoms, including numbness, tingling, and muscle cramps. Several factors can contribute to poor circulation. Atherosclerosis, the buildup of plaque in arteries, narrows the blood vessels, reducing blood flow. Conditions such as diabetes can damage blood vessels and nerves, further impeding circulation. High blood pressure, obesity, and smoking are well-known risk factors that can harm blood vessels and hinder the circulatory system. In some cases, genetics can play a role, as a family history of circulatory issues may increase one's susceptibility. If your feet are cold for the majority of the day, it is suggested that you schedule an appointment with a podiatrist who can accurately diagnose poor circulation, and offer appropriate treatment methods.
While poor circulation itself isn’t a condition; it is a symptom of another underlying health condition you may have. If you have any concerns with poor circulation in your feet contact Dr. Blake Zobell of Utah. Our doctor will treat your foot and ankle needs.
Poor Circulation in the Feet
Peripheral artery disease (PAD) can potentially lead to poor circulation in the lower extremities. PAD is a condition that causes the blood vessels and arteries to narrow. In a linked condition called atherosclerosis, the arteries stiffen up due to a buildup of plaque in the arteries and blood vessels. These two conditions can cause a decrease in the amount of blood that flows to your extremities, therefore resulting in pain.
Symptoms
Some of the most common symptoms of poor circulation are:
- Numbness
- Tingling
- Throbbing or stinging pain in limbs
- Pain
- Muscle Cramps
Treatment for poor circulation often depends on the underlying condition that causes it. Methods for treatment may include insulin for diabetes, special exercise programs, surgery for varicose veins, or compression socks for swollen legs.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions, please feel free to contact one of our offices located in Richfield and Ephraim, Utah . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
Causes and Effective Treatments for Cracked Heels

Cracked heels, a common foot ailment, can be both unsightly and uncomfortable. These painful fissures occur when the skin on the heels becomes dry and thick, and loses its natural elasticity. While cracked heels may seem like a cosmetic concern, ignoring them can lead to infection or more severe issues if left untreated. Several factors contribute to the development of cracked heels. The primary cause is inadequate moisture, often made worse by dry weather, excessive foot soaking, or harsh soaps that strip the skin of its natural oils. Overweight individuals and those who stand for prolonged periods may also be more susceptible due to increased pressure on the heels. Treating cracked heels involves a multifaceted approach. Hydration is key, so moisturize your feet regularly with a thick, emollient foot cream. Exfoliate gently using a pumice stone to remove dead skin. Wear comfortable, well-fitting shoes with proper arch support to alleviate pressure. If you have developed cracked heels, it is suggested that you consult a podiatrist who may recommend prescription creams or therapies to address underlying issues.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact Dr. Blake Zobell from Utah. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact one of our offices located in Richfield and Ephraim, Utah . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Choosing the Right Running Shoe for Your Foot Type
Running may seem like a simple to do. However, running is actually a complex movement that puts stress on the ligaments, bones, and joints of the body. Selecting the correct running shoe is important for increasing performance and avoiding risk of injury. Running shoes should be selected based on your foot type. Considerations such as trail versus road shoes are important. Your foot type dictates the degree of cushioning, stability and motion control you require. The most accurate way to learn your foot type is to visit a local shop that specializes in running shoes. Professionals can measure your arch type, stride and gait and help you with your shoe needs.
The design of running shoes is created around the idea of pronation. Pronation is the natural rolling movement of your ankle from the outside to inside when your foot strikes the ground. If you run properly you strike the ground on the outside of your heel and roll in the direction of your big toe before pushing off once more. Pronation is beneficial because it assists the lower half of your body in absorbing shock and storing energy. Those considered neutral runners pronate correctly and do not need running shoes that help correct their form. Neutral runners can choose from a wide variety of shoes, including barefoot or minimal types. However, those who have arch problems or who adopt an incorrect form while running may experience too much or too little pronation. They may require running shoes that offer additional support.
Those who overpronate experience an over-abundance of ankle rolling. Even while standing, those who severely overpronate display ankles that are angled inward. It is not uncommon for them to have flat feet or curved legs. The tendency to overpronate may cause many injuries. Areas that tend to become injured are the knees, ankles, and Achilles tendon. If you find that you have a tendency to overpronate, you should look at shoes that provide extra stability and motion-control. Motion-control shoes are straight and firm. Shoes of this type do not curve at the tip. The restricted flexibility along the middle of the shoe prohibits the foot from rolling too far inward as your foot strikes the ground.
A less common problem is underpronation. Underpronation, also called supination, is when the feet are unable to roll inward during landing. Those who underpronate have feet that lack flexibility and high arches. This prevents any kind of shock absorption, even though it does place less rotational stress on ankles and knees. This added force can cause fractures, ligament tears, and muscle strains because the legs are trying to compensate for the impact. Those who underpronate need shoes with more cushioning and flexibility. If you have a tendency to underpronate, selecting stability or motion-control shoes may cause you more problems by continuing to prevent pronation.
Selecting the Ideal Shoe for Running

Choosing the right running shoe is essential for an enjoyable and injury-free run, regardless of your running style. For road running, opt for cushioned shoes that provide ample shock absorption and support for consistent, even surfaces. Trail running demands shoes with a sturdy outsole, strong traction, and added stability to handle uneven, rugged terrain. If you are interested in sprinting and short-distance runs, lightweight shoes with spikes or cleats offer the grip and speed you need. For long-distance running, prioritize comfort, arch support, and ample cushioning to endure the extended impact on your feet. Minimalist shoes are designed for runners seeking a barefoot-like experience, promoting a natural stride and strengthening foot muscles. Understanding your running style and the surface you'll be running on will guide you in finding the perfect pair that complements your unique needs and preferences. If you would like more information about the type of running shoes to purchase for various running styles, it is suggested that you consult a podiatrist who can provide you with the information you are seeking.
If you are a runner, wearing the right running shoe is essential. For more information, contact Dr. Blake Zobell from Utah. Our doctor can provide the care you need to keep you pain-free and on your feet.
Choosing the Right Running Shoe for Your Foot Type
To increase performance and avoid the risk of injury, it is important to choose the right running shoe based on your foot type. The general design of running shoes revolves around pronation, which is how the ankle rolls from outside to inside when the foot strikes the ground.
- Neutral runners are able to choose from a wide variety of shoes, including minimalist shoes or even going barefoot.
- Runners who overpronate, or experience an over-abundance of ankle rolling, should choose shoes that provide extra motion control and stability.
- Runners who underpronate, or supinate, have feet that have high arches and lack flexibility, preventing shock absorption. They require shoes with more flexibility and cushion.
If you have any questions please feel free to contact one of our offices located in Richfield and Ephraim, Utah . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Arthritis Can Cause Pain in the Feet and Ankles
Flatfoot
Flatfoot is a foot disorder that is not as straightforward as many people believe. Various types of flatfoot exist, each with their own varying deformities and symptoms. The partial or total collapse of the arch, however, is a characteristic common to all types of flatfoot. Other signs of flatfoot include:
- “Toe drift,” or the pointing outward of the toes and the front part of the foot
- The tilting outward of the heel and the tilting inward of the ankle
- The lifting of the heel off the ground earlier when walking due to a tight Achilles tendon
- Hammertoes
- Bunions
One of the most common types of flatfoot is flexible flatfoot. This variation usually starts in childhood and progresses as one ages into adulthood. Flexible flatfoot presents as a foot that is flat when standing, or weight-bearing. When not standing, the arch returns. Symptoms of flexible flatfoot include:
- Pain located in the heel, arch, ankle, or along the outside of the foot
- Overpronation, or an ankle that rolls in
- Shin splint, or pain along the shin bone
- General foot aches or fatigue
- Pain located in the lower back, hip, or knee
Your podiatrist will most likely diagnose flatfoot by examining your feet when you stand and sit. X-rays may be taken to define the severity and help determine the treatment option best for your condition. Nonsurgical treatments can include activity modification, weight loss, orthotics, immobilization, medications, physical therapy, shoe modifications, and ankle foot orthoses (AFO) devices. If nonsurgical methods prove ineffective, surgery may be considered. Multiple surgical procedures can correct flatfoot; and depending on your specific condition, one may be selected alone or combined with other techniques to ensure optimal results.
Facts and Myths About Flat Feet
Flat feet, also known as pes planus, is a condition where the arches of the feet collapse, causing the entire sole to touch the ground. Contrary to common belief, flat feet are not always problematic or painful. Many individuals with flat feet experience no discomfort or other issues, leading active and fulfilling lives. However, some may face challenges such as foot pain or lower limb fatigue, especially if the condition alters their gait or posture. Flat feet can be hereditary, a result of injury, or develop over time due to wear and tear. Wearing proper footwear, practicing exercises to strengthen foot muscles, and using orthotic inserts can offer relief and support. Understanding the facts about flat feet can empower individuals to manage any associated concerns effectively and lead an active, healthy lifestyle. If you have flat feet, it is strongly suggested that you are under the care of a podiatrist who can help you to monitor this condition.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Dr. Blake Zobell from Utah. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact one of our offices located in Richfield and Ephraim, Utah . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
The Causes, Types, and Treatments of Achilles Tendon Injuries
Tendons are fibrous tissues that connect muscles with bone. The Achilles tendon is the largest tendon in the body. It connects the calf muscles at the back of the leg with the heel, and facilitates movements such as jumping, running, and walking.
Because the Achilles tendon is engaged so frequently and bears a great deal of pressure and stress throughout the day, it can become injured. Achilles tendon injuries cause the tissue to become irritated, inflamed, and swollen. Pain can come on gradually or be immediate, and will vary from mild to severe depending upon the injury. Where the pain occurs will vary as well, from just above the heel up through the back of the leg. There may also be stiffness in the tendon.
Achilles tendon injuries can often be caused by repetitive stress. They may also occur while running, playing tennis, gymnastics, football, basketball, dancing, soccer, baseball or other sports that require speeding up, slowing down, or pivoting quickly. Wearing high heels, falling from an elevation, stepping in a hole, having flat feet, bone spurs, tight leg muscles or tendons, wearing improper athletic shoes, exercising on uneven surfaces, or starting a new type of exercise can also cause Achilles tendon injuries.
The two most common Achilles tendon injuries are tendonitis and ruptures. Tendonitis causes painful inflammation and can occur in different parts of the tendon. Non-insertional Achilles tendonitis occurs when the fibers in middle of the tendon begin to break down, thicken, and swell. This condition typically affects younger, more active adults. Insertional Achilles tendonitis occurs where the tendon inserts into the heel bone. It is common for bone spurs to form with this type of injury. This condition can affect people of any age and level of activity.
Achilles tendon ruptures are a tear in the tendon. These breaks may be partial or complete. There may be an audible popping noise at the moment of injury and the pain will be sudden and severe.
An Achilles tendon injury can be diagnosed by your podiatrist after they examine you, check your range of motion, and possibly perform a calf squeeze test or review an X-ray or MRI. Depending on the type and severity of your injury, your podiatrist may treat your condition with rest/ice/compression/elevation (RICE), nonsteroidal anti-inflammatory medications, heel lifts, and stretching and strengthening exercises. If you have torn your Achilles tendon, treatment may include physical therapy, ultrasound, shockwave therapy, or possibly even surgery.